On 19 April 2024, Rishi Sunak set out his plans to tackle what he termed the “sick note culture” in the UK. This concept has been marinating in my mind since then, especially considering my personal experiences with mental health.
The term “sick note culture” is not only troubling but also reminiscent of past divisive rhetoric used by politicians. It raises serious questions about the government’s understanding and handling of mental health issues.
Sunak’s speech highlighted a significant rise in the percentage of people deemed unfit to work, from 20% in 2011 to 65% today. He argued that the current system writes too many people off, placing them on the wrong type of support with no expectation of finding a job.
While he acknowledged that those with debilitating severe conditions should not be expected to work, his focus on “low-level” issues being manageable through employer adjustments felt disconnected from the realities of mental health struggles.
This topic is deeply personal to me. Over the past two years, I have battled severe depression and PTSD, often feeling misunderstood and isolated. The notion of a “specialist” assessing my ability to work feels both intrusive and impractical. Mental health is a complex and fluctuating condition that cannot be adequately measured by a checklist or brief assessment.
For me, mental health issues are not just about feeling down; they encompass a range of symptoms, from heart palpitations and chest tightness to disrupted sleep patterns and overwhelming anxiety. These are invisible to an outsider and certainly not to a specialist without comprehensive training. The proposed solution seems to overlook the nuanced nature of mental health, risking further harm to those it intends to help.
In this post, I will explore the flaws in Rishi Sunak’s approach to addressing the so-called “sick note culture”. I will go into my personal experiences to highlight the impracticality of the government’s plan. Moreover, I will critically examine what a genuine mental health specialist would need to look like to effectively address these issues. By the end, it will be apparent that the current proposal is not only flawed but also potentially harmful to those genuinely struggling with mental health conditions.
My Personal Battle with Mental Health
My experience with mental health issues has been a challenging journey, deeply influenced by personal events. Over the past two years, I have struggled with severe depression and PTSD. One of the most significant recent triggers was receiving distressing news about my children.
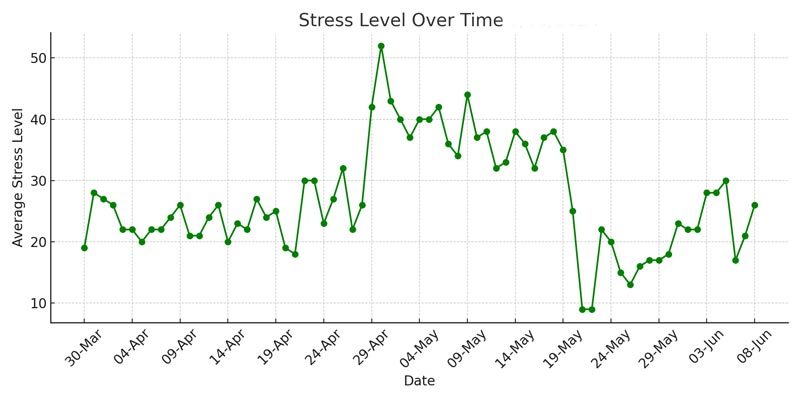
This event caused a drastic spike in my stress levels, as shown in the “Stress Level Over Time Chart” above. The readings are taken from my Garmin watch, which I wear throughout the day and night to help me gain control over my physical and internal feelings. Initially, I managed to stay calm, but as time passed, my stability deteriorated. My stress readings skyrocketed, and it took me over a month to regain control. Establishing a strict daily routine involving walks, exercise, breathing exercises, and yoga was crucial in managing my stress and slowly bringing my levels back down.
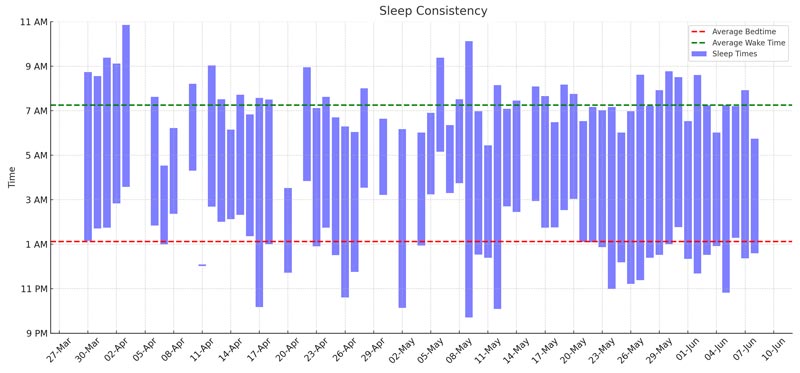
The impact of stress on my sleep was profound. The “Sleep Consistency Chart” above illustrates how my sleep patterns became highly irregular during this period of heightened anxiety. When my stress levels were at their peak, my sleep consistency suffered.
This inconsistency is a direct result of the so-called “sick note culture” failing to acknowledge the real and pervasive impacts of mental health struggles. Only after regaining control over my daily routines did I start to see some improvement in my sleep patterns. This chart vividly shows the correlation between my stress levels and sleep consistency, highlighting the importance of a stable routine in managing both.
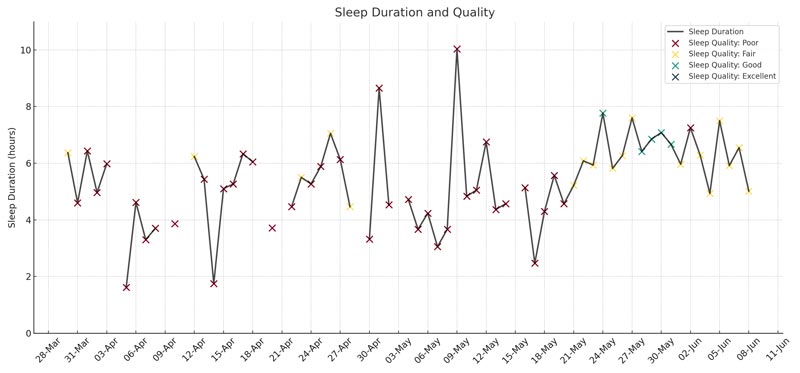
Additionally, the “Sleep Duration and Quality Chart” above provides a clear picture of how the quality of my sleep deteriorated despite sometimes achieving over six hours of sleep. You can see from the chart that I did not manage a single ‘excellent’ sleep quality, with only a handful of ‘good’ sleep. Most of my sleep in the two months was ‘poor’ quality.
The bad news about my children caused my sleep quality to plummet, with frequent awakenings, heart palpitations, chest tightness, and nightmares becoming everyday occurrences. This poor sleep quality severely affected my ability to function during the day. It demonstrates that even when sleep duration appears sufficient, the quality can be significantly compromised by underlying stress and anxiety.
These experiences highlight the complexities of mental health and how it cannot be easily measured or assessed. The so-called “sick note culture” approach fails to consider these intricacies. A specialist trying to gauge my ability to work would need to understand the intricate and fluctuating nature of mental health conditions.
To make an accurate assessment, this specialist would require extensive training/degrees across various disciplines, including medical, neuroscientific, physiological, and sleep studies. The charts above, generated from my Garmin watch data, provide insights that take time to be visible to an outsider. This data-driven approach is something a typical assessment might need to pay more attention to, leading to potential misjudgements about one’s capacity to work. I ask PM Rishi Sunak and his colleagues what this specialist you plan to train looks like?
By looking at these graphs, it becomes evident that mental health cannot be reduced to simple metrics or brief assessments. The proposed specialist system must be capable of understanding these nuances to avoid further harm to those genuinely struggling with mental health conditions.
The Government’s Dangerous Rhetoric on Sick Note Culture
The term “sick note culture” used by Rishi Sunak is troubling and reminiscent of past divisive rhetoric. It is reminiscent of Suella Braverman’s speech describing a “hurricane of migrants” coming to the UK.
The wind of change that carried my own parents across the globe in the 20th century was a mere gust compared to the hurricane that is coming.
Braverman admitted that politicians, including Conservatives, had failed to curb migration effectively and were too “squeamish” about being labelled as racist to bring order to the chaos. She warned that the “wind of change” that brought her parents to the UK was nothing compared to the “hurricane” of migration today, which dehumanises the issue and stokes fear.
Similarly, the use of “sick note culture” echoes the inflammatory language used by Enoch Powell in his infamous “Rivers of Blood” speech. Both instances involve framing societal challenges in a way that scapegoats vulnerable groups, be it migrants or individuals with mental health issues. This type of language is harmful and dangerously simplistic, reducing complex issues to soundbites that can mislead the public.
The rhetoric surrounding the “sick note culture” is harmful because it oversimplifies the realities faced by those struggling with mental health conditions. It implies that individuals exploit the system rather than acknowledge their genuine challenges. Victor Adebowale, Chair of the NHS Confederation, articulated this well when he said,
The language that we use… do we have a sick note culture? It’s cruel. You know it. If you’re at home and you… have long COVID, it’s a recognised illness as a result of the COVID. For every month you’re out of work, your mental health deteriorates.
Adebowale further explained that the term “sick note culture” fails to recognise the need for tangible support and empathy. He highlighted the importance of providing people with the help they need to regain confidence and skills rather than labelling them as part of a problematic culture. His comments emphasise that most individuals want to work and need appropriate support, not stigmatisation.
This type of performative language, as Adebowale calls it, lacks empathy and understanding. It does not consider the lived experiences of those with mental health issues, many of whom struggle invisibly. When the government uses such rhetoric, it risks creating punitive rather than supportive policies, ultimately causing more harm than good.
For me, the government’s use of the term “sick note culture” is not just a matter of semantics; it reflects a broader misunderstanding and misrepresentation of mental health issues. It is crucial to move away from such harmful language and towards a more compassionate and realistic approach to addressing mental health in the UK.
The Impracticality of “Specialists”
The feasibility of creating true mental health specialists, as proposed by the government, is highly questionable. During the Question Time panel on 25 April 2024, Chris Philp, the Minister for Policing, Crime, and Fire, needed help defining these specialists. His responses could have been more specific, indicating a lack of concrete plans. This raises significant doubts about the practicality and effectiveness of such specialists.
Chris Philp mentioned that these specialists would be trained to identify what people can do rather than just signing them off as sick. However, the process of creating these specialists could be more transparent. How can the government ensure these specialists have the comprehensive training to accurately assess complex mental health conditions? This remains a significant concern.
A lady in the crowd, a nutritional and lifestyle coach, highlighted the impracticality of this idea with a powerful example. She spoke about her client, who could not sit or stand for any length of time for over 18 years. Despite this, he was deemed fit to work based on a brief assessment. She pointed out the dangers of such superficial evaluations. She stated:
How are you going to train these experts when actually for me to assess one client takes me about eight hours?
Current and past assessment methods have consistently proven to be flawed. These methods often rely on brief, superficial evaluations that fail to capture the true extent of an individual’s condition. Mental health is complex and variable, influenced by numerous factors that a short assessment cannot adequately address. The lady in the crowd’s experience with her client underlines this issue, showing how a quick assessment can lead to incorrect conclusions.
Furthermore, another audience member discussed how mental health professionals often have to take on roles beyond their expertise due to systemic issues. They become housing officers and social workers, handling problems that GP’s cannot manage due to overwhelming workloads. This illustrates the multifaceted nature of mental health care, which cannot be addressed by a single type of specialist.
My own experiences further highlight these issues. When I completed my PhD in Engineering in 2009, I endured the frustrating process of job centre assessments. Despite my high-level qualifications, I was often told to apply for any job, regardless of its relevance to my field.
The people assessing me needed to gain the skills to understand my qualifications and the specific nature of my expertise. This demoralising experience highlighted the systemic failures in recognising and valuing advanced educational backgrounds.
Additionally, mobility assessments often fail as they are based on rigid checklists that do not account for fluctuating conditions. For example, the government previously had to reassess many cases where initial evaluations were superficial and did not capture the true nature of individuals’ disabilities. These past failures illustrate the systemic issues of relying on inadequately trained assessors to make complex determinations about health and capability.
The term “sick note culture” fails to recognise the intricacies of mental health. Practical mental health assessment requires a deep understanding of various medical, psychological, and social factors. Specialists would need extensive training across multiple disciplines, which is a monumental task. This complexity and variability make it impractical to develop a one-size-fits-all specialist.
The government’s proposal to create specialists to tackle the so-called “sick note culture” is fundamentally flawed. The current and past assessment methods have shown that superficial evaluations are ineffective. Mental health conditions are too complex and variable for a standardised specialist approach. A more comprehensive and empathetic system is required to address these issues adequately.
Broader Implications and Issues of Sick Note Culture
The discussion around the so-called “sick note culture” often highlights the systemic abuse of systems by both individuals and officials. Undeniably, some people exploit the system, including those in positions of power.
The MPs’ expenses scandal, in which numerous politicians were found to have claimed unjustifiable expenses, is a prime example. This scandal revealed that even highly qualified individuals who should know better can abuse the system for personal gain.
Furthermore, GP’s, overwhelmed with heavy workloads, might issue sick notes quickly to manage their time more efficiently. This practice can contribute to the perception of a “sick note culture.” Still, it is crucial to understand the context of these decisions. Overburdened GP’s might need more resources or time to conduct thorough assessments, leading to a system that can be misused.
However, it is essential to acknowledge that while there are always people who will exploit the system, this does not mean that the majority of claimants are doing so. The focus on systemic abuse should not overshadow the genuine needs of many individuals who rely on support due to legitimate health issues. Most people seeking sick notes or disability benefits are not exploiting the system but need genuine help.
Policies must be shaped with genuine empathy and understanding of individuals’ complexities. Instead of framing the issue as a widespread culture of deceit, it is vital to consider the personal struggles and systemic challenges that lead people to seek support. The narrative should shift from suspicion to compassion, recognising that the system’s primary purpose is to assist those in need.
Victor Adebowale, Chair of the NHS Confederation, during Question Time, pointed out that the language used around “sick note culture” is cruel and misleading. He emphasised:
For every month you’re out of work, your mental health deteriorates.
This highlights the need for policies that support rather than punish individuals, understanding that prolonged periods of unemployment can worsen mental health conditions.
Creating policies must address the root causes of why people need support and provide adequate resources for proper assessments. A system based on genuine empathy and a thorough understanding of individual circumstances is more likely effective and fair.
Overall, while it is essential to address systemic abuse, policies should not be punitive or based on the assumption that most people are trying to cheat the system. Instead, they should focus on providing comprehensive support, understanding the multifaceted nature of health issues, and ensuring the system works for those who genuinely need it.

Final Thoughts on Addressing Mental Health and Sick Note Culture
I believe that Rishi Sunak’s decision to target a segment of society with his “sick note culture” rhetoric was driven by internal party pressures. With significant in-fighting within his party and some members eyeing the Prime Minister’s position, coupled with unfavourable polls showing a 20-point deficit behind Labour, Sunak needed a strategy to galvanise support. Launching this initiative on 19 April 2024, just before announcing a general election on 22 May 2024 for 4 July, is a calculated move.
Throughout this post, we have explored the impracticality and potential harm of Sunak’s approach. As proposed, creating true mental health specialists lacks clarity and feasibility. The government’s past and current assessment methods must be revised, often relying on superficial evaluations. Mental health is far too complex and variable to be measured accurately by a one-size-fits-all specialist.
Proper mental health support is essential. It requires a comprehensive understanding of medical, psychological, and social factors, which cannot be captured through brief assessments or superficial metrics. My own experiences, supported by data from my Garmin watch, highlight how nuanced and personal mental health struggles are.
Rishi Sunak and his government must adopt a more compassionate and realistic approach to mental health. Policies should be based on genuine empathy, understanding the lived experiences of individuals, and providing the necessary support. Moving away from harmful rhetoric and towards a more supportive framework is crucial for the well-being of those genuinely struggling with mental health conditions. Only through such an approach can we address these issues effectively and humanely.


